Plenary Session 5 “Innovative concepts and new modalities of treatment in urothelial carcinomas” focused on topics such as systemic and intravesical therapies for Bacillus Calmette-Guerin (BCG)-naïve patients with high-risk non-muscle-invasive bladder cancer (NMIBC), and active surveillance (AS) in NMIBC. The session also featured a panel discussion on patient selection for conservative management of MIBC (muscle-invasive bladder cancer) after neoadjuvant chemotherapy. PhD researcher Dr. Verane Achard (CH), Dr. Javier Puente (ES), and urologist Prof. Morgan Rouprêt (FR) spearheaded the session.
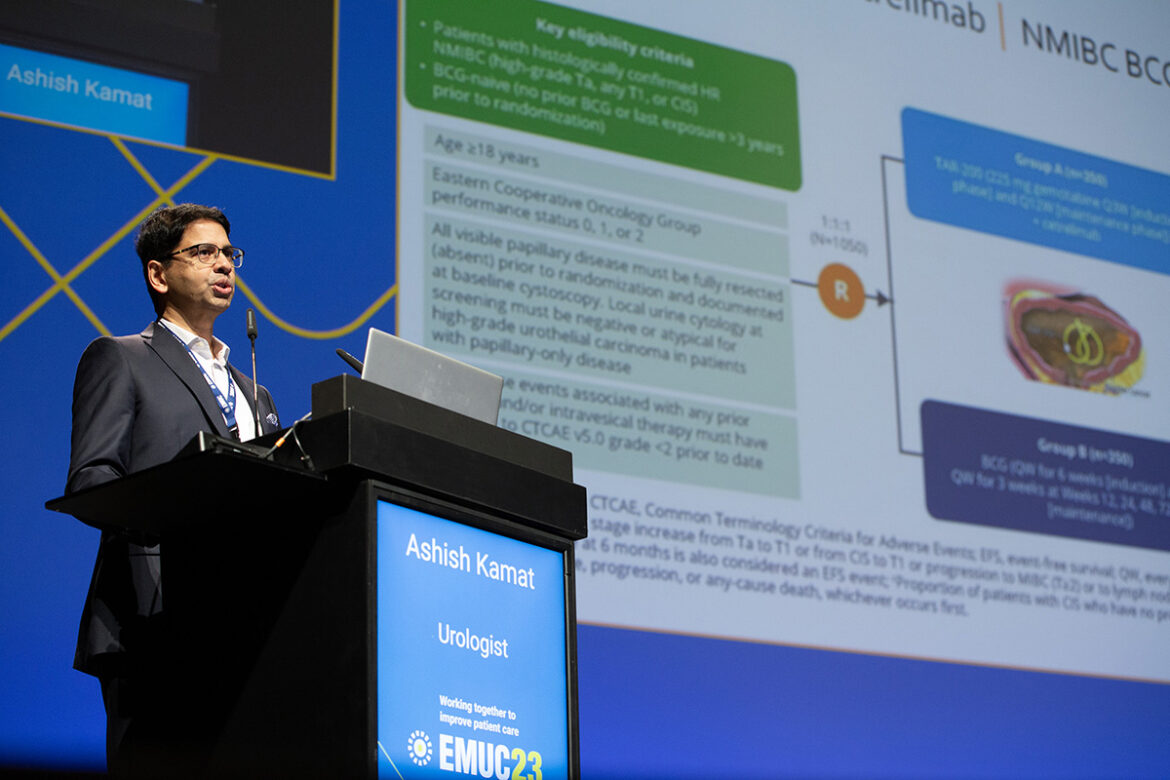
Prof. Ashish Kamat (US) presented “Systemic versus intravesical drug from high-risk NMIBC naive from BCG”. He stated, “The standard of care for high-risk, high-grade NMIBC is BCG. It reduces the risk of progression. If you use BCG as the standard of care, the risk progression drops from 9.6% to 5.8% for high-risk NMIBC, and from 40% to 14.8% for very high-risk NMIBC.”
Systemic vs. intravesical therapies
Prof. Kamat also enumerated the therapy options for patients with NMIBC: intravesical (e.g. intravesical chemotherapy, enhanced drug delivery, vaccines, and gene therapy) and systemic (e.g. immunotherapy [IO], targeted therapy, radiation, and other).
To demonstrate when to consider BCG-naïve patients with high-risk NMIBC for systemic therapy. He provided a patient case of a 79-year-old patient who is a long-time smoker and has diabetes and hypertension. The tumour characteristics are as follows:
- Largest tumour cluster: 4 cm, widely invasive T1 high-grade (T1HG), with 5% micropapillary component
- Base of tumour: muscularis propria present, no tumour, carcinoma in situ (CIS) present
- Trigone tumour: 2 cm, T1HG, no CIS, no muscularis propria present
- Bladder neck/prostatic urethra: with CIS, stroma present, not involved
Prof. Kamat explained, “Clearly, this is the type of patient you’d recommend for radical cystectomy. However, if the patient refuses the procedure and is worried about systemic disease, combining a systemic agent such as IO with an intravesical therapy such as BCG makes the most sense. This is the kind of patient where I would consider adding systemic therapy and not just intravesical therapy. In my opinion, it’s not a debate between intravesical or systemic therapies, but when to optimise the best treatment for the patient.”
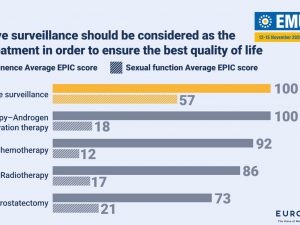
Active surveillance (AS) in NMIBC
AS in NMIBC is “lagging behind schedule” according to Prof. Paolo Gontero (IT). In his lecture “Active surveillance in NMIBC: myth or reality?”, he stated that there are less than 1,000 published cases in over 20 years.
Prof. Gontero pointed out that patients with recurrent low-grade Ta-NMIBC are the ideal candidates as there is a broad population of these potential candidates. He added that the accuracy of patients’ selection and follow-up may be hampered by suboptimal estimation of grading/staging and unreliable markers. Furthermore, current exit criteria are efficient but need to be more relaxed. There is negligible progression event and the duration is short.
Concerning NMIBC, the anticipated course for AS includes longer follow-up because the long-term impact of AS on the disease is still unknown. Prof. Gontero added, “Patients’ acceptance should be explored. There should also be a reduction of the unreliability of visual tumour appearance. In this respect, we can record videos of the procedures. We should also test AS against a competitive comparator such as office fulguration or chemoablation in the future.”
View the session recap and watch the full presentations on the EMUC23 Resource Centre.